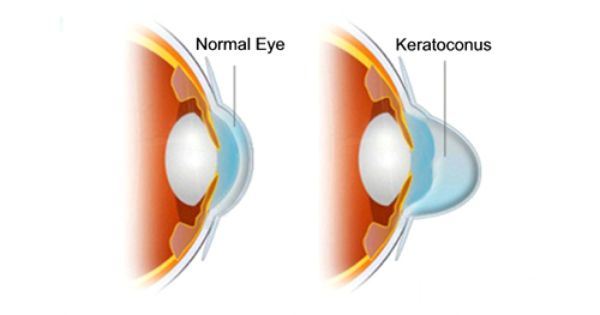
Keratoconus is a progressive condition of the eye that generally develops in younger people. It affects around 1 in 2000 people in the general population, and in males and females equally. The term 'keratoconus' means 'conical cornea' — referring to the shape of the cornea, the front surface of the eye, developing into a irregular cone shape due to progressive tissue thinning (ectasia).
Typical age of diagnosis is between 16 and 30. While it commonly affects both eyes, it may develop earlier or faster in one eye. Cases of keratoconus that develop at an earlier age (around adolescence) are usually more aggressive in progression.
Typical age of diagnosis is between 16 and 30. While it commonly affects both eyes, it may develop earlier or faster in one eye. Cases of keratoconus that develop at an earlier age (around adolescence) are usually more aggressive in progression.
SYMPTOMS & SIGNS
Symptoms of keratoconus can include blurred vision, ghosting, flaring, halos around lights and distortion of vision. Occasionally early cases can be misdiagnosed (by inexperienced or ill-equipped practitioners) as short-sightedness or simple astigmatism. An instrument that can detect keratoconus and monitor its progression is a corneal topographer (pictured below) which precisely measures the shape of the cornea and produces a computer-generated 3D topographical map of its contours. Changes in the shape of the cornea can be detected over time. We use our corneal topographer routinely when we suspect a patient may have potential distortions or irregularities in their cornea.
Symptoms of keratoconus can include blurred vision, ghosting, flaring, halos around lights and distortion of vision. Occasionally early cases can be misdiagnosed (by inexperienced or ill-equipped practitioners) as short-sightedness or simple astigmatism. An instrument that can detect keratoconus and monitor its progression is a corneal topographer (pictured below) which precisely measures the shape of the cornea and produces a computer-generated 3D topographical map of its contours. Changes in the shape of the cornea can be detected over time. We use our corneal topographer routinely when we suspect a patient may have potential distortions or irregularities in their cornea.
CAUSES
There are genetic and environment causes for keratoconus. Studies have indicated that about 20% of keratoconus cases have a hereditary basis. It is thought that people with keratoconus have a weakness in the collagen fibres forming the structure of the cornea, causing it to distort in shape.
There is also a link between keratoconus and excessive chronic eye rubbing in people with atopic conditions such as hayfever, allergies, eczema and asthma who may frequently have itchy eyes. We always recommend avoidance of eye rubbing as it may exacerbate the condition.
There are genetic and environment causes for keratoconus. Studies have indicated that about 20% of keratoconus cases have a hereditary basis. It is thought that people with keratoconus have a weakness in the collagen fibres forming the structure of the cornea, causing it to distort in shape.
There is also a link between keratoconus and excessive chronic eye rubbing in people with atopic conditions such as hayfever, allergies, eczema and asthma who may frequently have itchy eyes. We always recommend avoidance of eye rubbing as it may exacerbate the condition.
TREATMENTS
GLASSES
Keratoconus treatments are aimed at improving functional vision. Glasses may help to partially improve vision in the early stages and milder forms of the disease, but due to the irregular distortion of the cornea, keratoconus cannot be fully corrected with regular glasses lenses and some degree of blurriness or ghosting usually remains. As the cornea distorts further with disease progression, glasses are unlikely to provide satisfactory vision.
CONTACT LENSES
Most moderate cases of keratoconus can be effectively treated with special rigid contact lenses. These hard contact lenses give much better vision than glasses as the lenses mask the abnormal and irregular corneal shape and provide a new, smooth optical surface to allow the light to focus correctly into the eye.
There are three types of rigid lenses available — conventional rigid-gas-permeable (RGP) corneal lenses, hybrid contact lenses (featuring a rigid lens centre with a soft outer skirt), and large-diameter scleral lenses (and mini-scleral lenses) that cover the entire cornea and overlap onto the sclera (the white part of the eye surface).
Hybrid contact lenses and scleral lenses are fast growing in popularity around the world as the lenses of choice for individuals with keratoconus as they are more comfortable to wear than small-diameter RGP lenses. Scleral lenses are also more suitable for advanced cases of keratoconus, can reduce the risk of corneal scarring, and in many cases can even help delay or avoid the need for a corneal graft.
These types of rigid lenses are best fitted by speciality contact lens practitioners equipped with a corneal topographer and customised lens fitting sets. All of the above contact lens options for keratoconus are available here at Eyecare Concepts Melbourne, fitted by our experienced contact lens optometrist.
SPECIALIST TREATMENTS
Advanced or rapidly progressive cases of keratoconus may be treated by an ophthalmologist (eye specialist) with methods such as corneal collagen cross-linking, Intacs corneal ring segment implants, and if all other treatment options are unable to give a satisfactory visual outcome, corneal transplantation/graft surgery.
Corneal cross-linking (CXL) treatment helps to stabilise the strength and integrity of the corneal tissue to prevent further progression. In Australia, as of May 2018, individuals with documented progression of keratoconus may be eligible for Medicare-subsidised corneal cross-linking treatment. The effectiveness of the CXL procedure means many keratoconus patients can now avoid needing a corneal graft in the future.
It is worth noting that CXL is aimed at halting the disease progression of keratoconus rather than restoring clear vision. Patients who have undergone CXL will still require vision correction, usually in the form of contact lenses such as RGP, hybrid and scleral lenses.
Advanced or rapidly progressive cases of keratoconus may be treated by an ophthalmologist (eye specialist) with methods such as corneal collagen cross-linking, Intacs corneal ring segment implants, and if all other treatment options are unable to give a satisfactory visual outcome, corneal transplantation/graft surgery.
Corneal cross-linking (CXL) treatment helps to stabilise the strength and integrity of the corneal tissue to prevent further progression. In Australia, as of May 2018, individuals with documented progression of keratoconus may be eligible for Medicare-subsidised corneal cross-linking treatment. The effectiveness of the CXL procedure means many keratoconus patients can now avoid needing a corneal graft in the future.
It is worth noting that CXL is aimed at halting the disease progression of keratoconus rather than restoring clear vision. Patients who have undergone CXL will still require vision correction, usually in the form of contact lenses such as RGP, hybrid and scleral lenses.
If you have been diagnosed with keratoconus or an irregular cornea, ask us how we can help monitor your eyes for progression and treatment options available to correct your vision.
As an advanced contact lens practitioner in Melbourne, our optometrist is highly skilled at fitting corneal RGP lenses, hybrid contact lenses and scleral lenses for your eye condition.
As an advanced contact lens practitioner in Melbourne, our optometrist is highly skilled at fitting corneal RGP lenses, hybrid contact lenses and scleral lenses for your eye condition.
For further information or support, you can also visit the Keratoconus Australia website: www.keratoconus.org.au
We would also encourage you to join the Keratoconus Group on Facebook, which currently has over 16,000 members from around the world, including individuals with keratoconus and international eye care experts, sharing their personal experiences of their eye condition and various treatments. It's a great community and an excellent source of information.
https://www.facebook.com/groups/keratoconusgroup/
We would also encourage you to join the Keratoconus Group on Facebook, which currently has over 16,000 members from around the world, including individuals with keratoconus and international eye care experts, sharing their personal experiences of their eye condition and various treatments. It's a great community and an excellent source of information.
https://www.facebook.com/groups/keratoconusgroup/
Maintaining healthy eyes is key to good vision.
If you have noticed any vision changes, you need an eye check up.
Eyecare Concepts | The Myopia Clinic © 2017-23
KEW EAST | MELBOURNE
KEW EAST | MELBOURNE