|
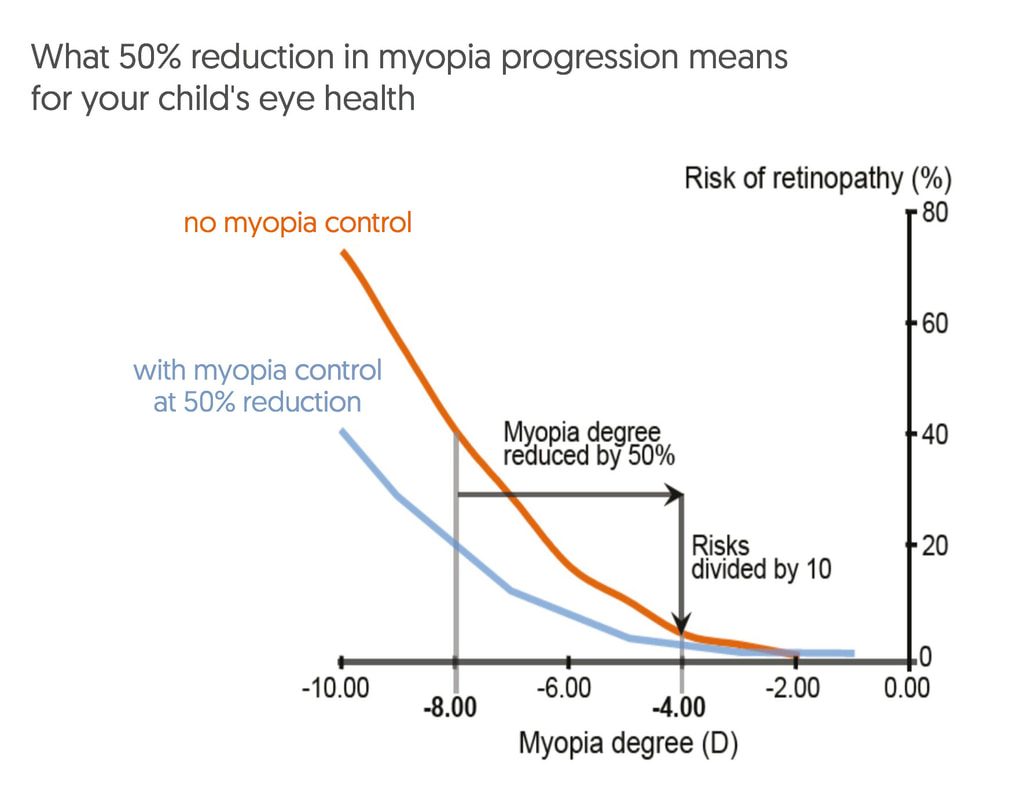
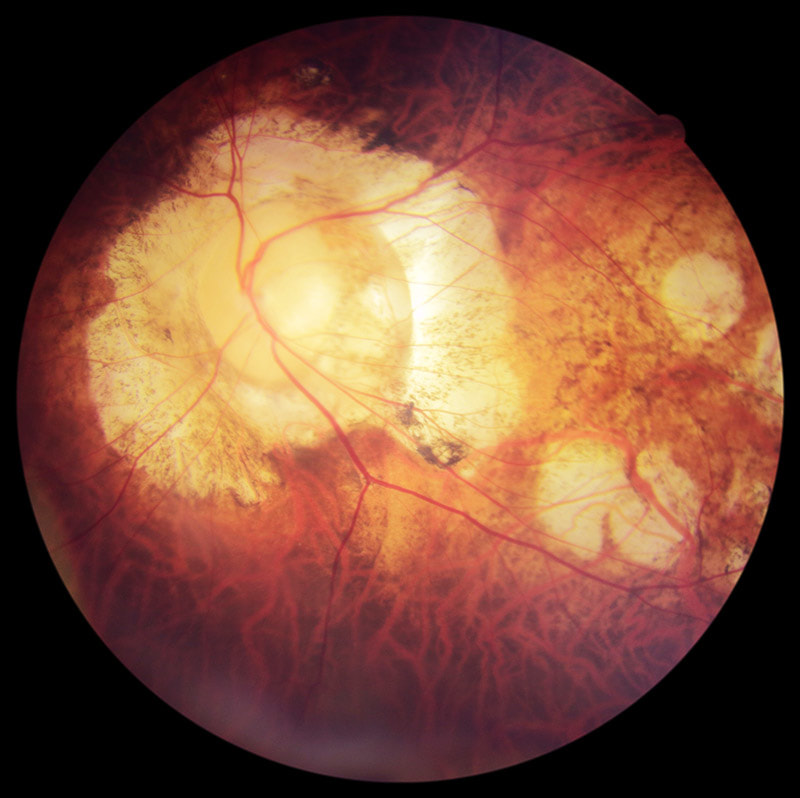
Parents often wonder how accurate children's eye tests are. That's understandable because young children often don't respond the same way as adults do during an eye examination. Children can find it harder to tell the difference between lenses presented to them when the optometrist asks, "Which is better? 1 or 2?". But an optometrist with experience and expertise in testing young children will be able to test children's eyes accurately. Paediatric eye examinations require a different set of skills and equipment than regular adult eye tests, and also more patience on the part of the optometrist. Being able to maintain a child's interest and attention are important to getting the most from their eye test. At Eyecare Concepts Optometry, we take the following steps to ensure that children who come to us for their eye care are well looked after and that their eye tests are as accurate as possible: LONGER CONSULTATION TIMES As an independent optometrist we can choose to spend more time with our patients. For children we allocate 40 minutes for their eye test. This gives the child time to settle in an unfamiliar environment, feel more comfortable, and to allow the time to perform all necessary tests without rushing the child. We also spend time explaining our findings to the parents in detail. ACCURATE DIAGNOSTIC INSTRUMENTS Adults' eye test results are determined by subjective responses (what the patient says during the test) and in a child's eye test more weight is placed on accurate objective findings (what the optometrist sees). Objective results, and the interpretation of these results by a skilled optometrist, are a vital part of children's eye tests. That means we can measure a child's eyesight and prescription without needing 'correct' responses from the child. To do that our clinic is equipped with advanced instruments that are highly accurate, and our optometrist cross-references the findings between different instruments to give the best possible assessment of a child's vision. CHILDREN'S EYE TEST CHART For children who are still learning their alphabet, we have a range of children's eye test charts to assess their vision. These include paediatric symbols (Lea symbols chart), numbers, 'Tumbling E' and 'Landolt C' eye charts designed specifically for testing younger children. ALL TESTING BY THE OPTOMETRIST The optometrist is the best person to carry out all tests in a child's eye examination. This includes preliminary testing and eye imaging tests that many optical chain stores delegate to their support staff. By being involved in the entire eye test journey, an experienced optometrist can pick up on subtle signs and issues that may otherwise be missed. NO CHILD IS TOO YOUNG TO BE TESTED Some parents tell us they were sent away by other optometrists saying their child is too young to be tested. Our optometrist can assess children of any age, even infants as young as 6 months. All children should have a comprehensive eye test by the age 3 to ensure that any vision issues that may interfere with normal vision development are detected early. THE USE OF EYE DROPS WHEN NEEDED While eye drops are generally not required in a child's eye test, they are occasionally necessary to make a definitive diagnosis of a child's eye condition. We will let you know if eye drops are recommended during your child's eye test. This is a called a cycloplegic examination, when we temporarily numb the eyes' focusing muscles. This in-depth examination is helpful when a child's focusing varies significantly during testing, or when the possibility of a very high prescription or lazy eye is detected, or when it is necessary to check the back of the eye in greater detail through dilated pupils. BULK BILLING CLINIC Our clinic's eye tests are bulk billed. That means there are no out-of-pocket costs to have your child's eyes comprehensively tested by us. And we also welcome parents bringing their children here for a second opinion if they have been tested elsewhere but are unsure of the results or have doubts about the recommendations given. It's one of many reasons why families across Melbourne are choosing Eyecare Concepts for their children's eye care. If you have any questions about our children's eye test services here at Eyecare Concepts Melbourne, please contact us on (03) 9819 7695 to speak with our children's optometrist. Myopia control is a hot topic in current eye research, in a bid to find the best ways of preventing and slowing vision deterioration for today's generation of children growing up in our tech-filled world. Many studies have been conducted globally in the past several years to analyse and compare the effectiveness of different treatment strategies available to reduce the progression of myopia ('short-sightedness') in children and adolescents. Naturally, different studies will report different findings and figures for treatment effectiveness, depending on variables such as sample size, subjects and study methodology. Here's how the current myopia control strategies stack up across multiple studies, in terms of the percentage reduction in the rate of myopia progression (eg. 0% = no effect in slowing progression; 100% = stops progression completely): Ortho-K corneal reshaping lenses: 32-100% Atropine eye drops (including low & high dose): 30%-77% Low-dose atropine eye drops: 59% Dual-focus & multifocal soft contact lenses: 29-70% Multifocal glasses for children with specific near focusing issues: 37% Multifocal glasses across all myopic children: 12-17% Regular single-vision glasses & contact lenses: 0-5% Due to the variability of the findings from different studies, and also individual variability from child to child from natural biological differences, this is generally what I recommend to parents seeking a myopia control opinion for their children: The best forms of myopia control treatment are currently Ortho-K overnight lenses, low-dose atropine eye drops, and dual-focus daytime soft contact lenses. Ortho-K and dual-focus contact lenses are optical treatments, and atropine eye drops is a pharmacological treatment; they work in different ways. As a guide, all three have an average effectiveness of around 50% in slowing the rate of childhood myopia progression. Some children achieve better myopia control than a 50% reduction, some may even stop progressing altogether, and others may need combination treatment to achieve the best control for their myopia. And some kids respond better to one type of treatment than another. What does a 50% reduction actually mean for my child? 50% reduction in myopia progression means we halve their prescription increase each year compared to no treatment or simply wearing standard single-vision glasses or contact lenses. For a child whose prescription is increasing rapidly at -1.00 per year, that reduces to -0.50 per year with myopia control treatment. While it may not sound like much, it is hugely significant over a longer timeframe. Over an eight-year period, for example, from age 8 to 16, if a child's myopia increases at a average rate of -1.00 per year (the actual rate may be faster some years and less other years), this child could have -8.00 degree of myopia at age 16. Halving the progression means he or she has -4.00 of myopia instead. There is a significant difference in the child's lifelong eye heath risks between having -4.00 and -8.00 of myopia. The risks of eye diseases associated with high myopia, such as retinal detachment and myopic macular degeneration, increase exponentially rather than linearly. Halving the degree of myopia from -8.00 to -4.00 reduces the risk of retinopathy (diseases of the retina) by a factor of 10, as the following graph illustrates. For more information about myopia control treatment options, visit our dedicated website at www.themyopiaclinic.com.au
EYECARE CONCEPTS · THE MYOPIA CLINIC MYOPIA CONTROL OPTOMETRIST — MELBOURNE As an optometrist with a strong interest in preventing short-sightedness progression in children, it's not uncommon for me to have to explain to frustrated and sometimes even angry parents who have come to see me for a second opinion after receiving incorrect, misleading or conflicting advice from other optometrists about ways to manage their children's eyes from getting worse. Their frustration is completely understandable. Most parents want the best for their children, and that includes their eyesight. And most parents will trust the advice and information provided by their optometrist during their children's eye tests. Unfortunately, sometimes that trust is misplaced. I have had parents tell me that other optometrists never advised them there was any way to prevent their kids' eyes from worsening each year with increasing short-sightedness (myopia). For some parents, despite voicing their concerns that their children's eyes were deteriorating at a rapid rate every 6-12 months, were simply told to accept this as being a 'normal' part of growing up and that was nothing that could be done except to update their lenses to a stronger prescription. As a result of being misguided by their optometrists, many of these children have developed moderate to high myopia at a young age. One girl I saw recently, in particular, is now over -10.00D short-sighted at just age 16, with exponentially higher risks of developing a retinal detachment, glaucoma and other eye diseases for the rest of her life. Eye growth and the eye health risks associated with progressive myopia cannot be reversed. Even laser surgery will not help as the eye's internal layers are physically stretched and thinned. If only someone had told them about myopia control before. For these patients to feel let down by their previous optometrists is entirely justified. It's time to think about short-sightedness as more than simply a condition involving glasses. Myopia is, in fact, an eye health condition. One with potentially serious complications if let to progress on its own. Glasses and contact lenses merely mask the underlying condition by making vision clearer. This is 2018, not 1990. Short-sightedness is a preventable condition today and has been for several years. Progressive vision deterioration in children and teenagers with myopia can be slowed down with clinically effective, evidence-based treatments. Optometrists who do not discuss myopia management strategies with the parents of children developing myopia are, in my view, failing to provide proper clinical care. And any optometrist who suggests "there's nothing that can be done to slow myopia progression in children" is either lying, incompetent, or at worst, negligent. The published clinical research papers on myopia control are widely available, and as eye care professionals all optometrists owe their patents a duty of care to provide the best care based on the best knowledge available. Ignorance is not a defence. My approach in this clinic is to give every child a full assessment of their visual functions and an analysis of their myopia progression and risk profile. I explain what this means to their parents and give them my professional recommendations based on the latest research applicable to their child's situation. I allow ample consultation time for parents to understand the information presented and to answer any questions they may have. For more challenging cases, I also reach out to world-renowned myopia experts on an international forum to discuss the appropriate management approach. My aim is always to ensure that parents are empowered with the knowledge to make a properly informed decision for their child's eyes. Here are some of the reasons why I think many optometrists in Australia today still do not discuss myopia control with their patients, or provide conflicting information:
LACK OF KNOWLEDGE Despite the availability of published evidence to support myopia management options for children, including effectiveness statistics of the various treatment strategies, many optometrists are unaware of these studies, or are lacking in their understanding of how to apply the relevant research data to clinical practice. Granted, myopia management is not a simple area of practice and is constantly evolving as new research is published. Keeping fully up-to-date demands attention and time. Many of the theories and knowledge surrounding myopia development and progression are also complex, that optometrists who are not specially interested in the subject matter may find it too complex to understand and to apply. BUSINESS MODEL It is unfortunate that many of today's optometrists operate under corporate business models that prioritise the selling of glasses over providing thorough clinical eye care. Pushed to see an many customers as possible, optometrists in these retail settings generally have shorter allocated consultation times of just 15-20 minutes (compared to 40 minutes at this clinic), which is often inadequate to perform highly detailed children's vision assessments, let alone discuss the available treatment options with the parents. Many optometrists working in retail-focused glasses stores consider myopia management as 'too difficult' and 'too time-consuming', therefore preferring to take the easy way out which is to simply prescribe a new pair of stronger glasses for their patients and send them on their way. Also, these corporate practices tend to employ many different optometrists, each with varying levels of skills, experience and knowledge, which inhibits proper continuity of care between visits when a patient may see a different optometrist each time and potentially may receive different, conflicting advice from one practitioner to the next. BIASED RECOMMENDATIONS An optometrist can only recommend to their patients services and products that they can offer in their practice. This is one reason why some parents receive contradictory advice at different practices while seeking a second opinion. For example, not all optometrists are therapeutically endorsed, which means they may not be qualified to prescribe medical treatments such as atropine eye drops for myopia control. Other optometrists may not have the technology or the expertise to fit Ortho-K lenses. Many optometrists do not have access to MiSight 1 Day contact lenses as they are only available to selected practices. For these reasons an optometrist's recommendations may be biased by what he or she can offer, hence the sometimes inconsistent advice from one practice to another. Multifocal glasses — despite being the least effective form of myopia management strategy — are often recommended by optometrists who are unable to, or reluctant to, to offer their patients potentially more effective options (such as atropine, Ortho-K or dual-focus soft lenses). I would suggest that if a practitioner has a child with rapidly progressive myopia in their room but is unable to offer the best solutions to help control the child's progression, it is in the child's best interests to be referred to another practitioner who can. At a dedicated myopia management clinic such as this, where every evidence-based treatment strategy is available, patients can be sure that recommendations are unbiased. COMMERCIAL CONSIDERATIONS The selling of glasses forms a large part of an optometry practice's revenue. So consider for a moment the business implications of treating a child to prevent their eyes from getting worse — if their eyes don't get worse the optometrist doesn't get the opportunity to sell them a new pair of glasses or new lenses every 6-12 months! There is actually a financial disincentive for practices that build their business primarily on selling glasses to offer myopia control to their patients. Prescribing treatments instead of glasses would increase 'chair time', increasing the number of reviews that do not generate glasses sales. As eye care professionals, optometrists should offer what is in their patients' best interests, but unfortunately many practitioners are driven by meeting company KPI targets and attracted to lucrative bonuses to drive sales. As utterly selfish and unethical as that seems, regrettably that is the commercial reality in today's increasingly retail-driven health care environment that most optometrists find themselves in. A further point to consider is that when a patient's prescriptions increases with their progressive myopia, the cost of their glasses lenses also increase. Many retail optometrists capitalise on selling lens upgrades — high-index thin lenses — for their medium and high prescription patients. There are even KPI targets specifically on up-selling lens upgrades — I would know, having previously worked for corporate optometry stores at various stages of my career. Keeping a patient's prescription low with myopia management means reduced dispensing of expensive high-index lenses over the individual's lifetime. Multiply that by tens of thousands of patients, and millions around the world. You can start to see why many mainstream optometrists do not proactively recommend myopia control to prevent children's prescriptions from increasing — despite the obvious risks to their patients' eye health as their myopia progresses. They have commercial reasons not to. At Eyecare Concepts, you can be assured that commercial considerations never come before patient care. That is what sets us apart. Colour vision deficiency (CVD), or otherwise called colour blindness, is a fairly common condition in the population. Around 8% of males (1 in 12) have some level of deficiency in colour matching, and around 0.5% of females (1 in 200). It is mostly a hereditary eye condition through a gene carried on the X chromosome (passing from mother's side), resulting in an imbalance of the numbers and densities of colour receptor cells (cones) in an individual's retina. Our eyes have three types of cone photoreceptors cells (green, red and blue) to detect colour information in our vision. There are two main types of hereditary colour vision deficiency: deutan (green cone receptor deficient) or proton (red cone deficient). A third type, tritan (blue cone deficient), is usually an acquired rather than congenital condition and is very rare. In each of these types, an individual may have a mild deficiency (almost normal), a moderate or a severe colour vision defect (significant difficulty in differentiating between certain shades of colours). At Eyecare Concepts, in addition to the standard Ishihara colour vision screening test (coloured dots forming numbers on a page) that most optometrists use, we have a more detailed colour vision test known as the Farnsworth D-15 colour matching test. While the common Ishihara screening tool can detect the presence of a colour vision defect, it does not differentiate between the type of colour defect or its severity. With the Farnsworth D-15 test — which involves matching a series of coloured discs from one to the next in similarity — we can assess the type of colour vision deficiency (deutan, protan or tritan) and also grade the severity of the deficiency between normal-mild, medium or severe. This is important when colour vision assessment is required for certain vocations or career choices. If you or your child has a colour vision deficiency, or there is a known family history, see us for a more comprehensive colour vision assessment test. EYECARE CONCEPTS
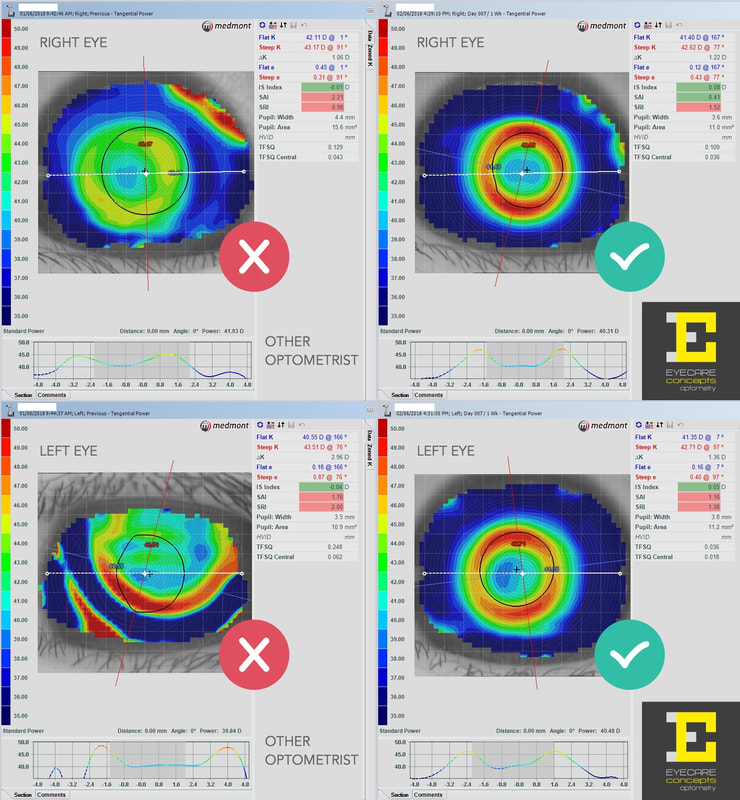
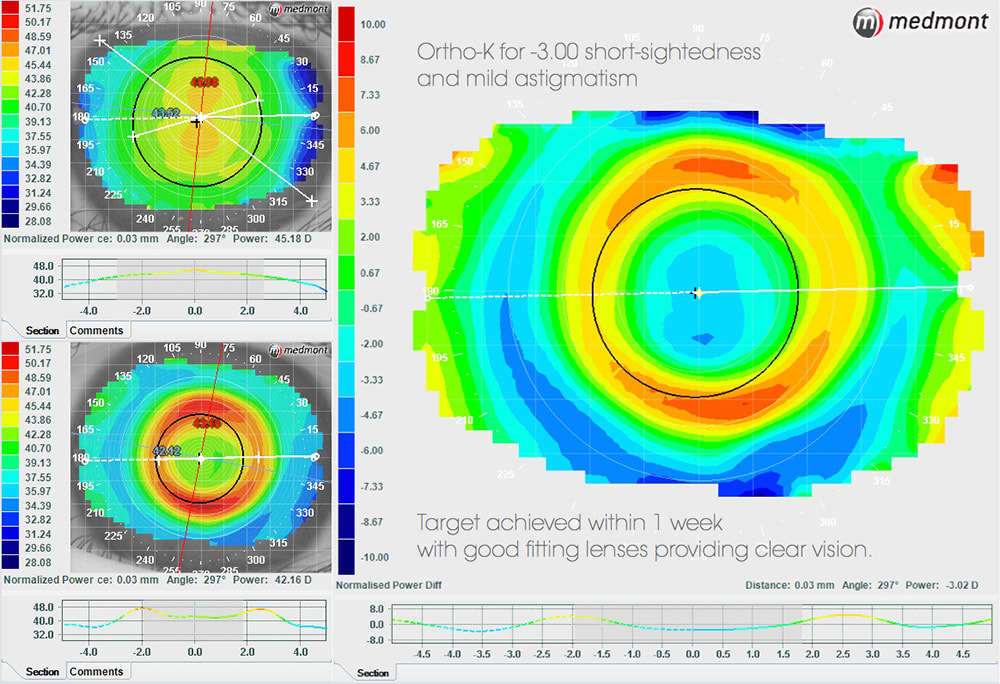
FAMILY & CHILDREN'S OPTOMETRIST — MELBOURNE If you or your child is wearing Ortho-K sleep contacts and they aren't working as well as expected, perhaps we can help. Fitting Ortho-K lenses is much more complex than regular contact lenses and requires a high level of professional skill, expertise and technology to get right. At this practice I have seen some patients with Ortho-K lenses fitted by other practitioners who may not have the best equipment or knowledge, resulting in sub-optimal vision and unhappy experiences. Below is an example of a 9 year old girl (-4.00 short-sighted) who was fitted with Ortho-K lenses by another Melbourne practice. She had never been satisfied with her vision from her lenses, experiences a large drop in vision from morning to evening, and despite her previous optometrist trying 4 different sets of lenses from 3 lens manufacturers she was unable to achieve 20/20 vision, hindering her vision at school. So her mum decided to seek a second opinion. At her first visit to this practice I measured her eye surface topography and it was quite obvious that her Ortho-K lenses were not fitting her eyes properly, hence the poor visual outcome and short treatment holding time during the day. Her treated vision was 20/40, that's 3 lines worse than 20/20 vision on the letter chart. Her lenses were unstable and de-centred on her eyes (especially the left eye) as she slept with her lenses on at night. Lens centration and treatment zone centration are key to achieving good results with Ortho-K. A well-centred Ortho-K lens places even pressure and forces across the eye surface for optimum moulding effect — essential for good vision and myopia control. I asked her to discontinue her lens wear for one week, by which time her cornea (the front surface of the eye) had completely reversed to its normal, non-treated shape. I then designed a new set of Ortho-K lenses for her using our advanced corneal topography technology and lens design software. This more sophisticated lens design approach allows me to create fully-customised lenses to suit all individual eye shapes and prescriptions. Having full control of every parameter of the lens shape, curvature and size means better fitting lenses and vision outcomes than older, trial lens-based Ortho-K fitting systems that some optometrists use. Within 2 weeks the new Ortho-K lenses were presented to her. At her first review, after one night of wear, she was already seeing better than her previous troublesome lenses, and one week later (when the above right-side topography maps were taken) she was achieving 20/20 vision and much happier with her vision at school. It is expected that the quality of her vision will improve further still as she wears her Ortho-K lenses into her second and third weeks and the corneal moulding and treatment zone areas stabilise. So a very happy patient and mum and well worth the visit to see us! Dr Philip Cheng — Melbourne Optometrist & Orthokeratologist
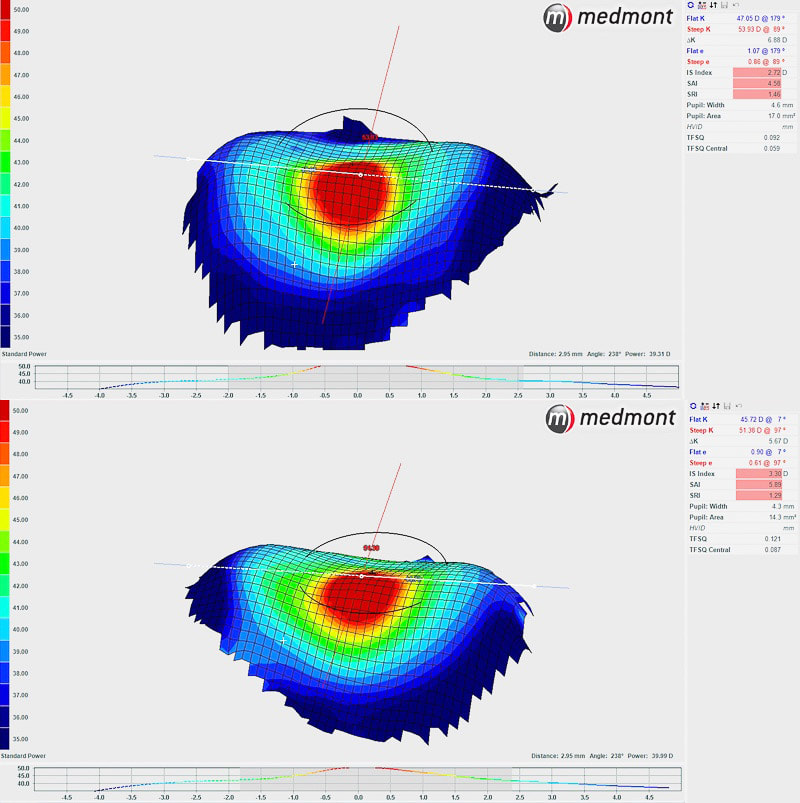
Member of the Orthokeratology Society of Oceania (OSO) Naturally, when people have blurry vision they think they might need glasses. And yes, in many cases, glasses may be all they need to fix their blurred vision after having a thorough eye examination at an optometrist. Sometimes, however, glasses cannot fix a person's blurred vision, at least not entirely. Most of the time this may be due to age-related eye changes such as cataracts, glaucoma and macular degeneration, but occasionally it can also happen to younger people. Recently I had in my practice a young patient who came in for a second opinion about his eyes. He had seen an optometrist in a shopping centre a little while back and was prescribed glasses for the first time there. He was concerned that his vision was still blurry even with his glasses on. After taking a detailed history I proceeded to test his eyes, and soon it became apparent to me what his eye issues were and why he was still having problems with his vision. He had a condition called keratoconus ('cone-shaped cornea') — a progressive eye condition that causes the front surface of the eye, the cornea, to become thin and distorted. Unlike normal astigmatism (unequal eye surface curvature across two meridians, like an egg shape), which is very common, in keratoconus the eye surface is vastly uneven and irregular. That means light entering the eye is scattered in many different directions, and not focused at a point or in one plane. This eye surface irregularity means the lenses in the glasses he was prescribed with cannot fully correct his vision deficit and blur, as glasses can only bend (or refract) light in up to two meridians. Unfortunately he wasn't explained this by his previous optometrist. It's possible the other practice didn't have the instrument to properly diagnose his condition. We use an instrument called a corneal topographer to accurately measure the shape of the eye surface when we suspect a case of keratoconus or other conditions that cause distortions in the cornea. With the data captured we can instantly produce a 3D topographical map of the cornea, as illustrated below, to show the contours of the eye surface and any irregularities present. This instrument is also used for advanced contact lens fitting, Ortho-K and dry eye analysis. What can be seen in the images below (of the right and left eyes) are areas of surface distortion, with a steep area (in red) resembling a cone shape. This is a classic case of keratoconus. With this condition, the best way for him to see clearer (than what is possible with glasses) is to wear special rigid contact lenses, to effectively provide his eyes with a new, smooth optical surface. These specially made contact lenses are individually designed for each eye using the 3D topography maps, to ensure of ideal fitting lenses on the distorted eye surfaces. EYECARE CONCEPTS — ADVANCED EYE CARE & CONTACT LENS PRACTITIONER — MELBOURNE
This follows from my last eye blog, Ortho-K: How Does It Work? How long does Ortho-K take to correct vision?The length of time it takes for Ortho-K overnight lenses to fully correct your vision will depend on your pre-treatment prescription and your individual eye shape. Other factors include quality and length of sleep each night (7-8 hours is ideal), consistency in wearing the lenses regularly, rigidity of the eye surface layers, the cornea, that can vary from person to person, lens design parameters, pupil size, presence of and amount of astigmatism to be corrected and the curvature of the eye surface. In my practice, all our Ortho-K patients have enjoyed significant improvement in their vision even after just one night of lens wear. Typically a patient with a medium level of short-sightedness, say -3.00 dioptres of myopia, will have over half of this prescription (around -2.00D) corrected already at their first review, in the morning following their first overnight wear of the lenses. By the end of week 1, he or she will have about 85% (around -2.50D) of their prescription corrected, and this further improves in the 2nd week to achieve 6/6 or 20/20 vision. Some patients experience faster vision correction progress, and some slower — this is normal as each individual's eyes are different. Some optometrists or websites may claim to be able to achieve 20/20 vision after one night of Ortho-K — while this may be possible in some cases with a simple prescription, I prefer my patients to have a realistic expectation of their treatment progress and outcome. As part of our Ortho-K Package for first time wearers we can provide, where needed, a spare pair of glasses made with a mild correction to help you see clearly during your first few weeks of Ortho-K treatment. This pair of glasses is also helpful for those who wish to wear their Ortho-K lenses every 2nd or 3rd night, instead of every night. As the treatment effect begins to wear off the glasses help to support their vision until they resume Ortho-K lens wear. Ortho-K vision correction is flexible, not everyone will need to wear their lenses nightly, depending on their personal vision needs and the holding time of their Ortho-K treatment. Individuals with astigmatism (uneven eye surface curvatures) tend to take a little longer to reach optimum vision. This is because the corneal reshaping involved in an eye with astigmatism is more complex. Astigmatism is corrected using customised dual-axis Ortho-K lenses. Some patients have astigmatism in one eye and not in the other, and these patients often will have faster vision correction in the eye without astigmatism, and with about 1 week difference between the two eyes in reaching the optimum vision outcome. Higher levels of short-sightedness (high myopia of over -6.00D) will also take longer for good visual outcome to occur, as greater amounts of eye surface flattening is required. Typically around 3 weeks for full or close-to-full correction is my advice to patients with high myopia considering Ortho-K lenses. During this initial period when treatment effect is gradually building we supply temporary soft contact lenses in steps of decreasing power to support the individual's daytime vision. With higher prescriptions it is normal for an individual to experience some ghosting and halos around lights, particular in dim conditions and at night. This usually improves with time as the Ortho-K treatment effect increases across a wider area on the eye surface. With very high prescriptions (eg. -8.00D short-sighted) it may not be possible to fully correct vision to 20/20 due to lens and biological limitations, in which case the individual may be left with a residual amount of short-sightedness (eg. -1.00D after a correction of -7.00D with Ortho-K for a -8.00D individual). This is termed 'partial correction'. Many patients with very high prescriptions are happy with a partial correction as it already significantly reduces their dependency on glasses, and if they do need to see clearer they can wear a light prescription pair of glasses during the daytime, rather than their usual thick and heavy glasses. In summary, these are the typical timeframes for Ortho-K lenses to effectively correct vision in most individuals: Low level myopia (less than -2.00D) — 3-4 days. Medium level myopia (-2.00 to -4.00D) — 1 week. Moderate level myopia (-4.00 to -6.00D) — 1-2 weeks. High level myopia (more than -6.00D) — 2-3 weeks.  We monitor your Ortho-K progress closely with corneal topography measurements at each visit. In this patient, full correction and 20/20 vision is achieved at 2 weeks. We monitor your Ortho-K progress closely with corneal topography measurements at each visit. In this patient, full correction and 20/20 vision is achieved at 2 weeks. EYECARE CONCEPTS — ORTHO K PRACTITIONER — MELBOURNE
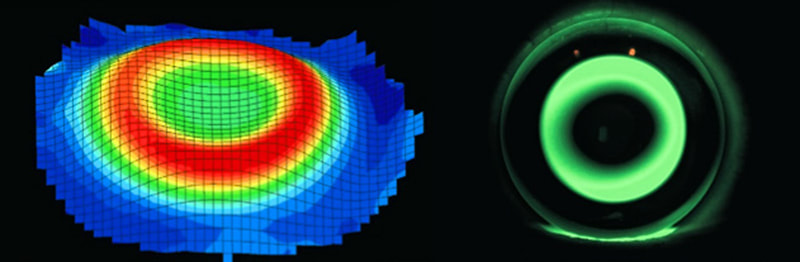
Ortho-K, short for orthokeratology, is a relatively new concept to many Australians. Most people may not have heard of it before, or know what it does, or how it works. If you're reading this page you probably want to learn more about Ortho-K and how it might help you or your child see clearer. In the next few eye blogs I will go into detail to explain everything you need to know about Ortho-K overnight contact lenses, which I believe is the future of vision correction. What is Ortho-K?Ortho-K is a special type of vision correction technology that uses a breathable rigid contact lens to change the shape of your eyes as you sleep. Also called Sleep Lenses or Night Contacts, you put on the lenses just before you go to bed, and when you wake up in the morning you remove your lenses and enjoy clear vision for the rest of your day, without wearing glasses or daytime contact lenses. How does it work? Ortho-K sounds amazing because it really is. Our Ortho-K patients find it incredible to get their clear vision back without needing to wear glasses or contacts during the day. No more dry eyes or discomfort at work, and for kids no need for the parents to worry about them losing their glasses or contacts at school. The science behind this technology is a little complex, but here's a brief explanation of how it works. For correction of short-sightedness (blurred vision in the far distance, also known as myopia), an Ortho-K lens flattens a central 5-6mm zone of your eye's front surface, the cornea. This surface flattening is similar to what happens with laser surgery (LASIK), only that Ortho-K is a temporary and reversible process and laser surgery is permanent. Flattening the cornea by a precisely calculated amount bends light to refocus it onto the surface of your retina, restoring your vision. An Ortho-K lens a specially designed rigid contact lens made to precisely fit the shape of your eye's surface. Every lens is tailor-made for each eye's shape and prescription. At Eyecare Concepts we use the sophisticated Medmont E300 corneal topographer (pictured below) with 102,000 individual points to scan your eyes' unique surface contours to generate 3D topographical maps of its shape. We then use this topography data and advanced computer simulation software to design your lenses to fit your eyes perfectly. The information we can capture is so precise that we can design the fitting of your lenses with an accuracy level measured in microns (0.001 mm). The image below shows how an Ortho-K lens works on the eye to correct vision. The lens, together with the eye's natural tear layer and eyelid in its closed state during sleep, places gentle hydraulic forces on the eye's surface, to gradually mould its shape by the precise pre-determined amounts required to give clear vision. You never feel any addition pressure on your eyes while wearing the lenses during sleep as the forces are very gentle. The centre of the lens does not actually directly touch the centre of the eye's surface but rather it vaults over the centre, and supported by a very thin film of tears, by approximately 20 microns (0.02 mm) — less than half the thickness of a strand of human hair. This is the kind of precision involved. The shape of an Ortho-K lens is different from other kinds of contact lenses. It is also technically known as a 'reverse geometry lens'. There are multiple curves on the back of the lens surface that create different pressure zones and for helping the lens to centre correctly on your eye as you sleep. The fluro-green areas on the right-side image show the areas where the shape of the lens changes from the central 'treatment zone' to the peripheral 'alignment zone'. This lens is fitting perfectly on the eye with a well-centred and even treatment zone, important for good, clear vision. The green glow is from fluorescein dye placed on the eye during the lens evaluation process. Normally the lens is completely clear. The left-side image is a 3D topography map of an eye following Ortho-K vision correction — showing flattening of the central zone of the eye surface (circular area in green), surrounded by a peripheral band (in red) of surface elevation changes which also helps to control short-sightedness progression in children and teenagers (myopia control) using Ortho-K lenses. Below is an example of one of our patients successfully fitted with Ortho-K lenses. The upper-left image is her natural eye surface shape before Ortho-K lens treatment. She had a prescription of -3.00 short-sighted plus a mild amount of astigmatism. The lower-left image shows the post-treatment shape of her cornea after Ortho-K lens wear. The red ring represents the positioning of her lens during sleep, showing excellent lens centration. On the right image the centre blue zone is the vision correction zone and is the ideal treatment effect that we are looking for. Her -3.00 prescription and astigmatism was fully corrected with Ortho-K, giving her 20/20 vision in just 1 week. EYECARE CONCEPTS — MELBOURNE ORTHO K PRACTITIONER
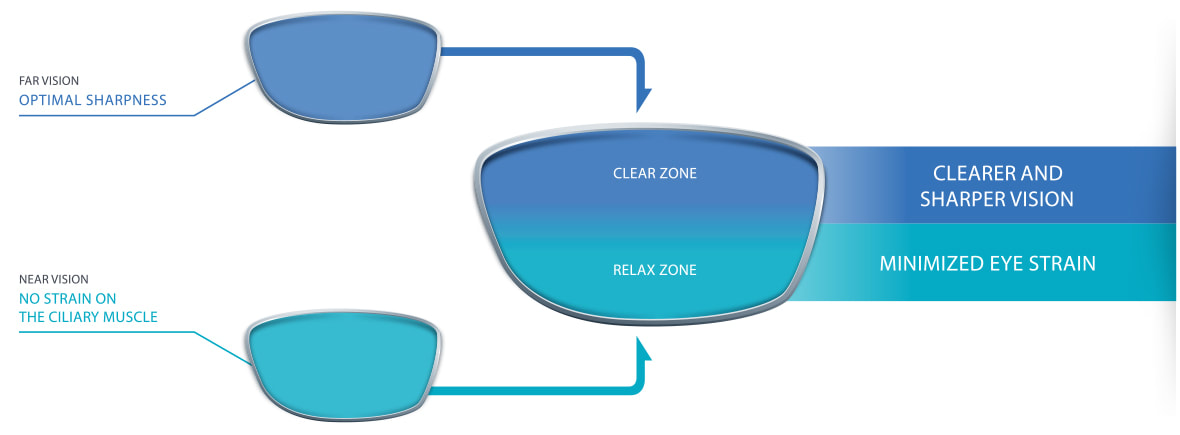
If this is you at work, you may have what is called Computer Vision Syndrome (CVS), or Digital Eye Strain. CVS is a common problem in our modern digital society where a large part of our days is spent staring at a computer monitor, on a laptop or tablet or using a smartphone, both at home and at work. CVS can affect up to 90% of people who spend more than 3 hours a day concentrating on digital devices. Typical symptoms of CVS include headaches, blurred vision, sore eyes, red eyes, tiredness, neck pain, difficulty refocusing from near to far and occasionally could also include dizziness and double vision. Why do we get Computer Vision Syndrome? Prolonged periods of focusing on a near object causes the eye's focusing muscles to become tired. For some people when this happens their eyes start to lose focus up-close, making near vision blurry. And when they try to focus even harder to read their computer screen they can end up straining their eyes and getting a headache. Or they may lean forward towards their screen and getting neck pain from improper posture. For other people, their far-distance vision can become blurred. This can occurs because their focusing system has become 'locked' at close-range, then when they look away into the distance their eyes are unable to relax, causing blurred vision. Some people can mistake this for 'short-sightedness' — where far-distance vision is always blurred relative to near — but in these cases it's actually the near work that causes the symptoms and far-distance glasses won't necessarily help. Some young adults, however, do develop true short-sightedness (myopia) from prolonged computer use. An experienced optometrist can distinguish between true short-sightedness and near-work-induced distance blur and recommend the most appropriate solution to the problem. Staring at a computer screen can often also cause dry eye. This is because when we stare at a computer our blink rate is reduced. When we don't blink frequently enough our eye surface becomes dry. Common symptoms of dry eyes are redness, irritation and burning sensation. Some people experience watery eyes, thinking if their eyes are watering they can't be dry, when in fact the cause of the watery eyes is actually dry eyes, as strange as it may seem. When our eyes become too dry and irritated they can start to produce tears as a reflex response. Dry eye can also be exacerbated by environmental factors such as air conditioning in summer and heating in winter. How to get help for Computer Vision Syndrome? If you have symptoms of CVS, the first thing to do is to book an eye test with an experienced optometrist for a comprehensive assessment of your eyes' focusing and eye health. Sometimes it can be a simple focusing issue such as slight long-sightedness (increased focusing effort at near) or astigmatism (irregular eye surface curvature) that a pair of prescription glasses with anti-reflective coating will make a big improvement to your symptoms. Often, a more specialised type of lens called an anti-fatigue lens will be what you need for your Computer Vision Syndrome. An anti-fatigue lens is like a mini-progressive lens with two power zones that help you relax your eyes when focusing up-close. Here at Eyecare Concepts, we offer the Essilor Eyezen and the Nikon Relaxsee anti-fatigue lenses, both specifically designed to relieve digital eye strain. The blue light protective coating of these lenses also help to reduce eye strain from brightly-lit digital devices. Our optometrist will recommend the optical solution tailored to your personal vision needs. Prescription glasses and anti-fatigue lenses are rebatable on your private health optical cover. For individuals with dry eyes, we can also assess your dry eye condition with our special instrument that analyses the quality of your tears and how quickly your natural tear film evaporates in-between blinks. With this analysis we can treat your dry eye condition more effectively. As a therapeutically-endorsed optometrist we can prescribe medicated eye drop treatments if necessary for more severe cases of dry eye. And if you have oily or blocked tear glands we have in-office eyelid warming therapy to treat the underlying cause of your dry eyes. EYECARE CONCEPTS OPTOMETRIST — KEW, BALWYN, BALWYN NORTH
Here at Eyecare Concepts, a family optometry practice with a focus on children's vision, I test a lot of kids' eyes. Kids of all ages and from different family backgrounds. Many children come in for their routine eye checkups and have normal eyesight and healthy eyes, which is always great to see. Some children’s cases are more challenging, but it’s very satisfying and professionally rewarding when I'm able to help them and enhance their lives with better vision. Lazy eye is a condition that most parents have heard of and are often concerned about. Sometimes the term ‘lazy eye’ gets confused with a turned eye or crossed eye. In optometry speak, lazy eye is called amblyopia, while a turned eye is called strabismus. They are often related, but quite different conditions. A lazy eye is usually a healthy eye but the eye and the brain are not working together properly. The visual processing system and nerve pathway associated with this eye is under-developed, from the brain becoming accustomed to 'ignoring' this eye in favour of the stronger eye. Without proper neural stimulation, the suppressed eye falls behind the good eye in eye-to-brain development. The majority of cases of lazy eyes in Australian children are associated with long-sightedness (hyperopia). Some children are born highly long-sighted in one or both of their eyes. A long-sighted eye is an eye that is physically shorter in length than normal, or has a lens that is too powerful, so that light entering the eye is focused behind the retina instead of on it. Most children are mildly long-sighted when young, that is perfectly normal, but when an eye is significantly long-sighted (usually +4.00 or above) the eye is unable to fully compensate for this and the result is blurred vision both in the distance and up close. Normal development of the visual system is hindered by blurred vision from the affected eye/s. A lazy eye can also result if a child has one eye that is significantly more short-sighted (myopic) than the other, or has a high degree of astigmatism (uneven eye surface shape). It is important to diagnose lazy eye in a child from an early age. Amblyopia occurs in around 2-3 in every 100 children, so it's not a rare condition. Some children have mild forms of amblyopia, and some have more severe forms. If a lazy eye is not detected, corrected or treated before age 8, permanently reduced vision in the affected eye can result and which will affect the child for the rest of his or her life. Lazy eyes are usually not treatable, or are extremely difficult to treat, in adulthood. Loss of vision in one eye means the child has impaired stereo (3D) vision and depth perception, and can affect potential future career ambitions as an adult, as some professions require good vision from both eyes. One tell-tale sign that your child may have a lazy eye is a turned eye (strabismus). An eye that is highly long-sighted will have a greater tendency to turn inwards toward the nose (termed esotropia), especially when the child is tired. Some children may have an eye that turns outwards (termed exotropia). An inward-turning strabismus is more common in Caucasian children, while an outward eye turn is more common in kids from Asian backgrounds. If you suspect your child may have a eye that turns or wanders, whether it affects one eye or both eyes, turns inwards or outwards, and even if it happens only occasionally, you should have your child examined by an eye care practitioner — an optometrist or an ophthalmologist — as soon as possible. With some infants and toddlers their eyes may give the appearance of being turned or crossed but are in fact straight. This is an optical illusion called pseudostrabismus caused by facial features and eyelids that are not yet fully developed. As trained professionals, we can differentiate between a true strabismus and a pseudostrabismus. We suggest seeking a professional opinion if you have any concerns at all about your child's eyes. Our recommendation is that all parents should bring their children to an optometrist for their first eye test by the age of 3, even if they show no signs or symptoms and seem to be perfectly fine. Young children do not realise anything is wrong with their sight, they are not aware of what blurred vision is, and can appear to be functioning perfectly, especially when a problem affects only one eye. Often it's only at their first eye test that significant issues are discovered. Children will usually have a basic vision screening test by their maternity nurse when they reach 3.5 years of age. This test is called the Melbourne Initial Screening Test (MIST). While these tests are helpful they are not always reliable and are not a substitute for a proper comprehensive eye examination. We believe all kids should be tested by an optometrist even if they have passed their screening test, for a more in-depth assessment of their eyesight, visual functions and eye health. In our children's clinic we have special instruments and sophisticated eye measuring equipment to test young children, and objective tests that do not require any responses from the child if they are too young to read letters, identify symbols or give reliable responses. We also use dilating eye drops to more thoroughly assess your child's eyes and focusing. The presence of a lazy eye, turned eye, long-sightedness, short-sightedness and astigmatism can be detected. Where a lazy eye is found we can diagnose the cause of it and implement a treatment plan to gradually build up the vision in this eye and to make both eyes work together as a team. This usually involves glasses (sometimes contact lenses), eye patching or eye drops, and vision therapy. With timely and appropriate treatment the visual outcome for a child with a lazy eye is usually very good. As an eye care professional, to see a child's face light up and smile when given glasses for the first time and being able to see better is always such a delight. And I'm reminded of what a privilege it is to have the opportunity, and to be entrusted with this responsibility, of looking after young children's eyes and enhancing their lives through eye care. EYECARE CONCEPTS
FAMILY & CHILDREN'S OPTOMETRIST — KEW, BALWYN, BALWYN NORTH |
AuthorPhilip Cheng - B.Optom (Melb) Ocular Therapeutics (GCOT). Optometrist at Eyecare Concepts Kew East, Melbourne. An experienced eye care & contact lens practitioner with expertise in myopia control & orthokeratology. Archives
August 2018
Categories
All
|
Eyecare Concepts | The Myopia Clinic © 2017-23
KEW EAST | MELBOURNE
KEW EAST | MELBOURNE












 RSS Feed
RSS Feed